A Proven Thumb Joint Replacement.
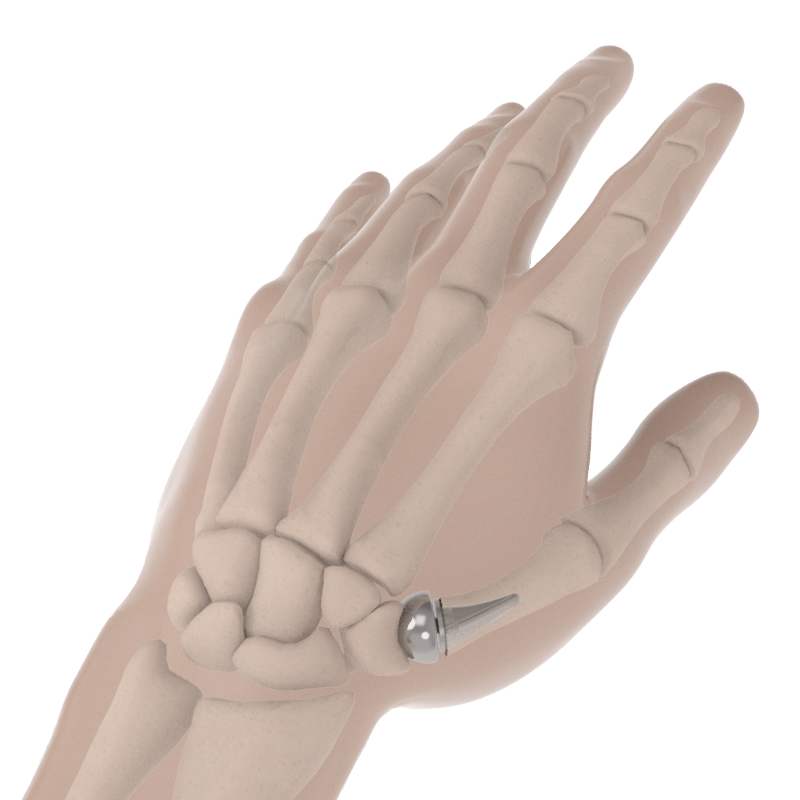
The BioPro Modular Thumb Implant is a two-piece implant designed to treat arthritis in the thumb (CMC) joint. Today, traditional surgical treatments involve removing the bone at the base of the thumb (trapezium), eliminating the thumb joint altogether. The BioPro Modular Thumb was designed to replace the joint, not remove it, providing patients with pain relief and faster recovery.1
Understanding Thumb Arthritis
The thumb joint is one of the most common sites of arthritis in the body, affecting up to 15% of the population older than 30 years old and up to 33% in postmenopausal women. The ability to perform tasks such as writing, opening jars, playing musical instruments, turning doorknobs and handling tools would not be possible without the thumb. Arthritis occurs when the smooth cartilage that covers the ends of the bones in the joint are damaged. When arthritis occurs in the thumb joint, it can cause severe pain, swelling, decreased strength, and motion. It often becomes difficult to do simple everyday tasks and the pain can become so severe that you may experience pain at night when sleeping.
Common symptoms
- Pain with tasks that require pinching or gripping such as opening a jar, turning a key, or pinching an object
- Swelling and tenderness at or around the base of the thumb
- Loss of strength
- Bump or enlargement at the base of the thumb
- Limited motion
- Dull aching pain after use
Diagnosis
If arthritis of the thumb is suspected, an X-ray can be taken to determine the amount of damage. From the x-ray the doctor will evaluate the joint space, alignment, and if any bone spurs (osteophytes) are present. The stage of arthritis and severity of the symptoms will determine the next step. It is usually treated with conservative care, however since arthritis is a progressive condition, it may worsen over time and surgery may be required.
Comparing Treatments
Since there is no way to replace the cartilage, surgical treatments address the condition by removing the bone-on-bone contact. The most common surgical treatment and the treatment often presented to patients involves the complete removal of the trapezium bone at the base of the thumb. The BioPro Modular Thumb Implant instead replaces the joint with a two-piece implant, giving your surgeon 48 different implant combinations to choose from, helping ensure a personalized fit.

- Replaces joint, forming a new socket into the trapezium
- Maintains thumb length and cosmetic appearance1
- Improves pinch and grip strength1
- Fast recovery1
- If pain persists, may be revised with a traditional surgery1

- Removes the base (trapezium) and suspends the metacarpal with a tendon from the forearm
- Shortens the thumb, changing the overall appearance of the hand2
- Initial decrease in pinch strength2
- Long recovery2
- If pain persists, revision surgery has been shown to lead to an even worse outcome3
Learn what treatments may be right for you.
Find a Surgeon
To locate experienced surgeons in your area, please complete the form to access our surgeon locator. Alternatively, you can email us at info@bioproimplants.com or call (810) 982-7777.
Consult with your surgeon
Discuss all your possible treatment options and expectations after surgery.
Undergoing joint replacement
Joint replacement surgery with the BioPro Modular Thumb Implant is an outpatient procedure. You should be in and out in one day and on the road to recovery.
Recovery
Below is the typical timeline for patients after undergoing a thumb joint replacement with the BioPro Modular Thumb Implant. Each patient’s recovery may be different. Please discuss your protocol with your surgeon prior to surgery.
2-4 weeks
A cast or splint will be worn while the thumb heals
4-8 weeks
Rehab or strength exercises
8-12 weeks
Resume normal activities and sports

The Implant Design
The BioPro Modular Thumb Implant is designed to provide a precise fit for each patient’s unique anatomy, with 48 different configurations available (four stems and twelve heads). Our comprehensive system includes specialized instrumentation for surgeons to accurately measure and trial implant sizes before final implant placement.
The standard implant is manufactured from Cobalt Chrome, a biocompatible metal with a long history of safe use in joint replacements. However, due to the small amount of nickel present in Cobalt Chrome, it may not be suitable for patients with nickel sensitivity. In such cases, we offer a Titanium alternative. We strongly recommend that patients discuss these options with their surgeon to determine the most appropriate choice for their individual needs.
Patient Stories
Dr. Duffner’s returns to surgery
Dr. Duffner, an orthopedic surgeon in Palm Springs, CA, was contemplating early retirement due to painful arthritis in both of his thumbs. Due to his past training as a surgeon, he was aware of the traditional treatments available but wanted an option that would help maintain his key pinch and grip strength. After undergoing the joint replacement procedure by Dr. Neil Jones, he returned to work. Listen as he shares his experience.
Ruth’s experience with both surgeries
After undergoing LRTI surgery on her right hand 12 years ago, Ruth recently received a BioPro Modular Thumb Implant in her left hand from John Faillace, MD (Galveston, TX). Listen as she shares and compares her experiences.
In the News
After suffering from osteoarthritis in both thumbs for more than 10 years, Carolyn decided to undergo the joint replacement procedure. “I have complete mobility, flexibility, and strength is coming back”.
Frequently Asked Questions.
- Pritchett JW, Habryl LS. A promising thumb Basal joint hemiarthroplasty for treatment of trapeziometacarpal osteoarthritis. Clin Orthop Relat Res. 2012 Oct;470(10):2756-63. doi: 10.1007/s11999-012-2367-7. Epub 2012 May 15. PMID: 22585348; PMCID: PMC3442003.
- Komura S, Hirakawa A, Masuda T, et al. Chronological changes in surgical outcomes after trapeziectomy with ligament reconstruction and tendon interposition arthroplasty for thumb carpometacarpal osteoarthritis. Orthop Traumatol Surg Res. 2020;106(2):357-364. doi:10.1016/j.otsr.2019.11.020
- Sadhu A, Calfee RP, Guthrie A, Wall LB. Revision Ligament Reconstruction Tendon Interposition for Trapeziometacarpal Arthritis: A Case-Control Investigation. J Hand Surg Am. 2016;41(12):1114-1121. doi:10.1016/j.jhsa.2016.09.005