MPJ Hemi Implants
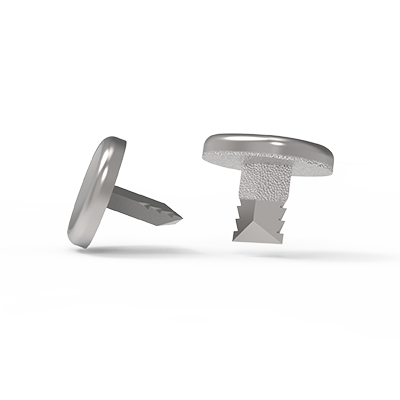
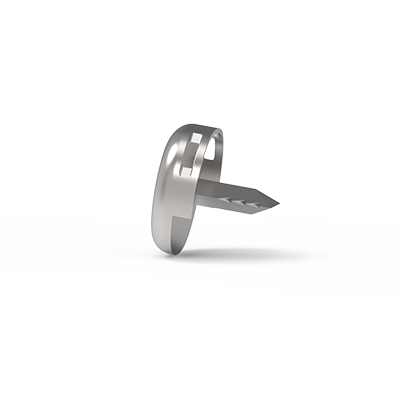
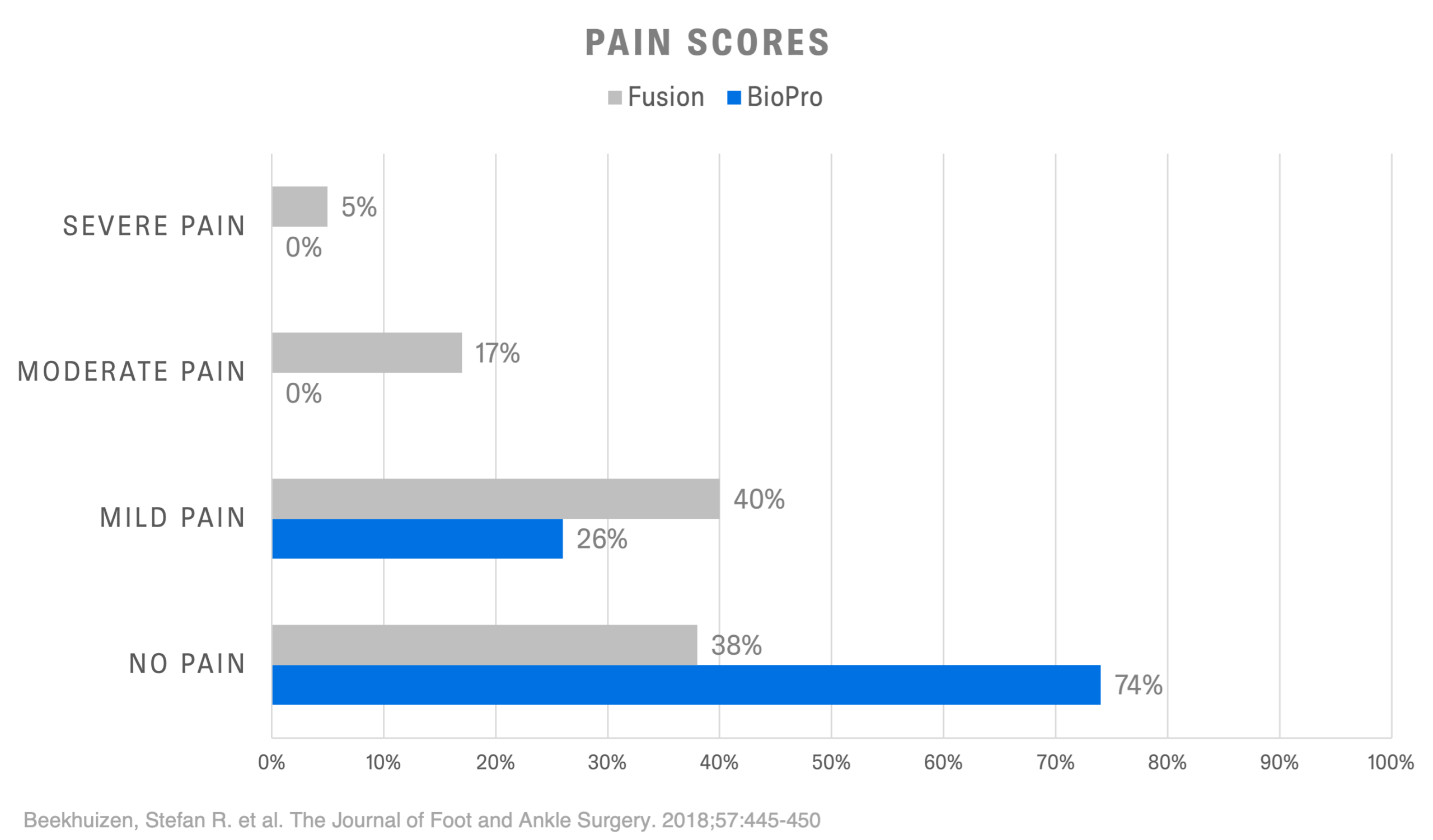
The BioPro® MPJ Hemi Implant is the only Hemi backed by 70+ years of clinical data. Our low-profile, press-fit implants are designed to replace the articular surface of the proximal phalanx in a painful, arthritic metatarsophalangeal (MTP) joint. The procedure offers restoration of motion and pain relief, with a minimal bone resection technique.1,2
- 20+ year survivorship data.1
- +95% implant survivorship on average.*
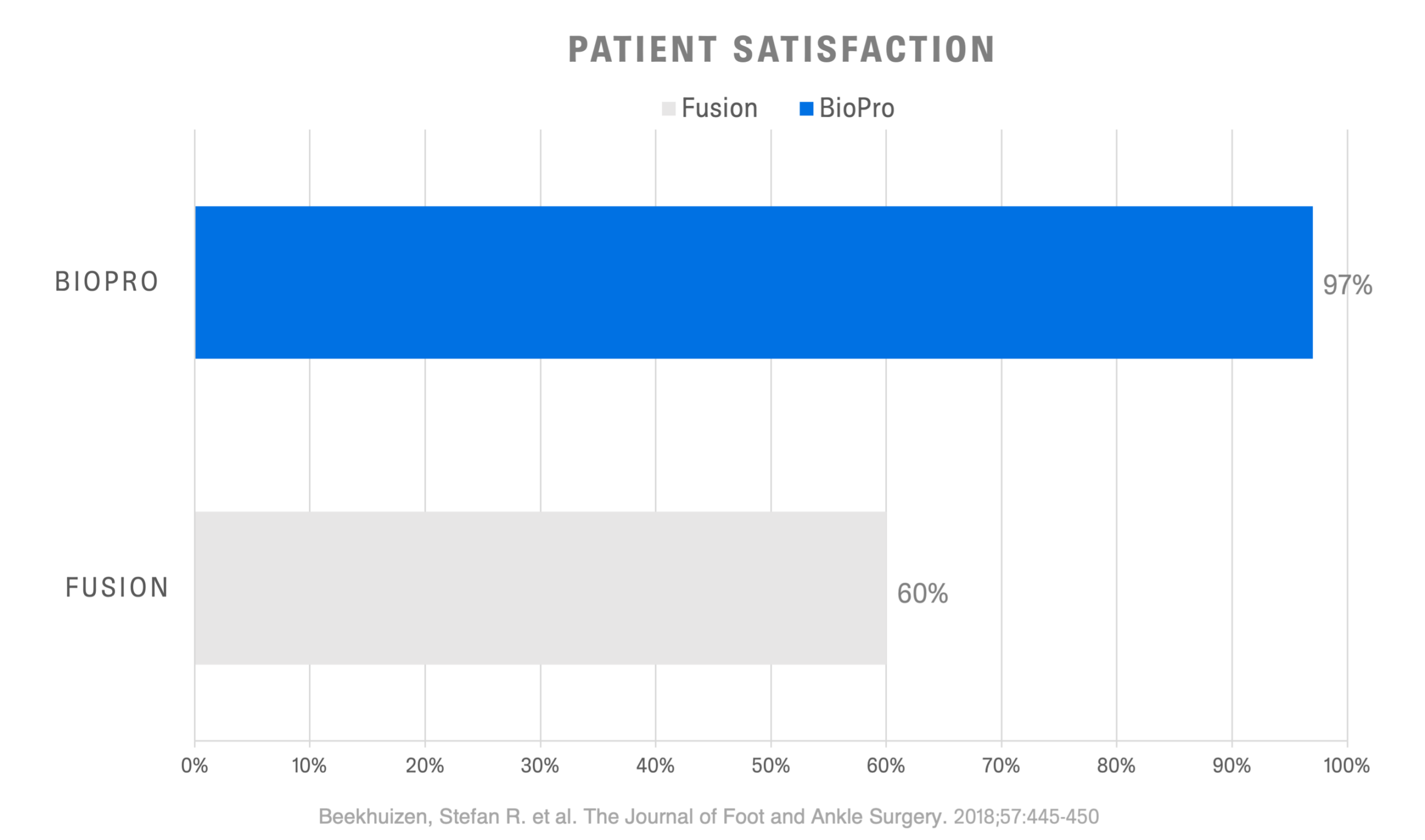
- 97% of patients would recommend the procedure.2
- Immediate weight-bearing.
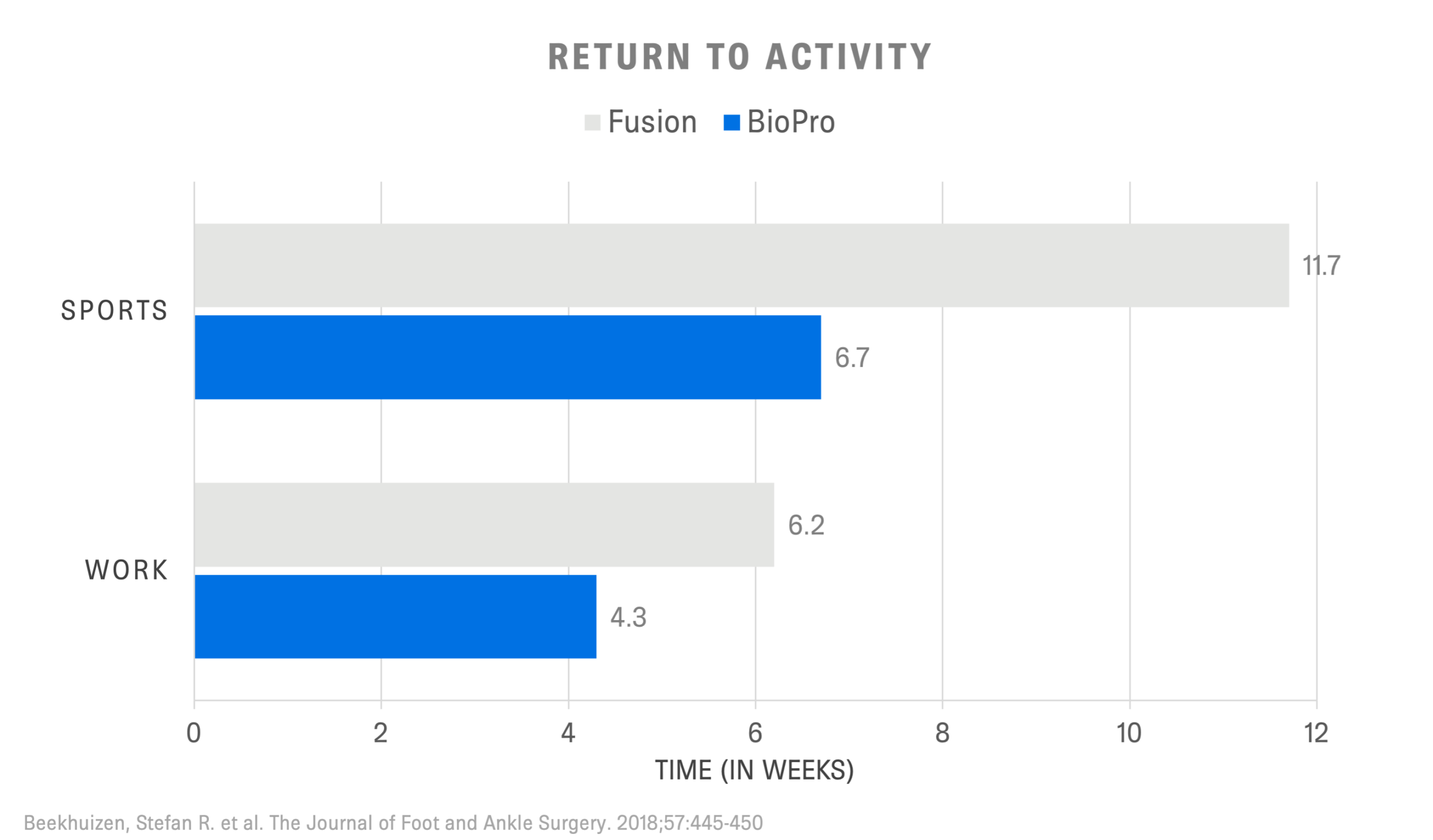
- ≤6 weeks return to activities.2
Related Videos
Surgical demonstration of the First MPJ Hemi Implant
Surgical demonstration of the Lesser MPJ Hemi Implant
Surgical demonstration of the HemiEDGE Implant
Related Documents
| Title | Type | Document Link | hf:tax:doc_type |
|---|
Find My Rep
REFERENCES
- Townley, MD, Taranow, DO. A metallic hemiarthroplasty resurfacing prosthesis for the hallux metatarsophalangeal joint. Foot & Ankle International 1994;15(11):575-80
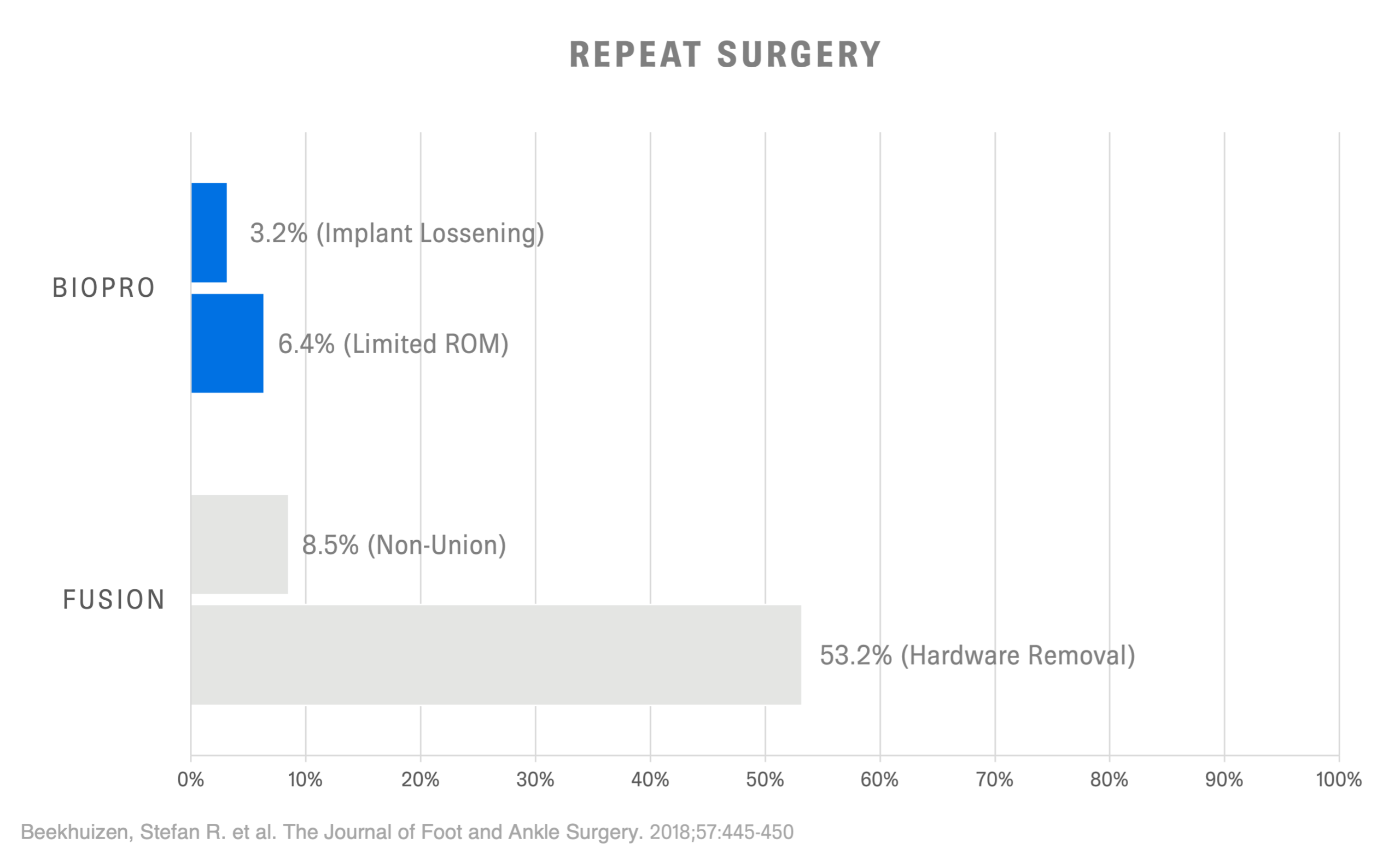
- Beekhuizen, Stefan R. et al. Long-Term Results of Hemiarthroplasty Compared With Arthrodesis for Osteoarthritis of the First Metatarsophalangeal Joint. The Journal of Foot and Ankle Surgery , Volume 57 , Issue 3 , 445 – 450
- Garras DN, Durinka JB, Bercik M, Miller AG, Raikin SM. Conversion arthrodesis for failed first metatarsophalangeal joint hemiarthroplasty. Foot Ankle Int. 2013 Sep;34(9):1227-32. doi: 10.1177/1071100713488093. Epub 2013 Apr 23. PMID: 23613329.
- Jacob, H.A.C. Forces acting in the forefoot during normal gait – an estimate. Clinical Biomechanics , Volume 16 , Issue 9 , 783 – 7922. 14.
- Palastanga, N., & Soames, R. (2012). Anatomy and human movement: structure and function (6th ed.). Edinburgh: Churchill Livingstone.